Current Research
Up-to-date HIV-related research.
Current Research
Up-to-date HIV-related research.
This section includes studies that have impacted medication use, care, and stigma related to HIV treatment. Treatment is highly effective and the earlier treatment starts the better the health outcomes. Consistent use of effective treatment is an important part of prevention and will reduce the risk of transmission.
If the virus is suppressed below 200 copies/mL or is undetectable on lab work there is zero risk of transmission to a sexual partner or transmission through pregnancy.
HIV medication
People living with HIV will be prescribed a combination of medications known as “antiretrovirals” to suppress the virus. The medications in these combos include different types/classes. The specific combination is decided upon several considerations by your health care provider and may include: drug resistance, drug interactions, side effects, patient preference, prescriber experience, and lab work results.
It is important to take your medication as prescribed by your physician. Newer studies are evaluating the importance of taking medication every day – but for now it is important to take exactly as prescribed until further evidence or told otherwise by your health care provider. If you are interested in current studies enrolling individuals in Canada visit: Catie Clinical Trials
Overview of Studies and Trials
These studies investigated if the use of an all-in-one pill combination with two medications in it would be effective for people new to HIV treatment. They found the medications were just as effective as the three-drug regimen compared against it. Fewer medications in treatment could potentially reduce potential side effects and drug interactions. However, the studies did not find improvements in safety during the trials compared to other regimens as both were tolerated equally.
Prior to this, two-drug treatment regimens were reserved just for individuals to possibly switch to if they first became undetectable on other treatment (see Sword 1 and 2 Studies below). This new regimen is now available and combines HIV medications that have already been on the market in Canada, known as lamivudine and dolutegravir.
This study investigated whether individuals who are virally suppressed on some 3-drug HIV treatment regimens could be effectively switched to a 2-drug regimen. The study found a regimen with lamivudine and dolutegravir could be effective for these individuals.
This study investigated if an alternative to the only official PrEP regimen in North America (emtricitabine, tenofovir disoproxil fumarate) would be effective. As a result of this study the FDA in the United States has approved an additional medication regimen for PrEP use. However, the study had limitations on ciswomen and is not currently indicated for that patient group.
The alternative regimen is not yet approved in Canada for PrEP but is in use as part of HIV treatment regimens. It includes emtricitabine like the current PrEP regimen, but has a different formulation of the second ingredient tenofovir. This updated version of tenofovir may result in less side effects related to bones and the kidney. Depsite this, our current PrEP regimen is generally well tolerated and major side effects are rarer with regular monitoring.
**Canada has just approved Cabenuva for monthly injections: https://viivhealthcare.com/en-gb/media/press-releases/2020/march/viiv-healthcare-announces-first-global-regulatory-approval-of-ca/
The study is investigating if a two-drug long-acting injectable medication is as effective as current treatments for people living with HIV and the virus is already suppressed on treatment. The results have been promising and we will likely see the medication become available in 2020.
Once available individuals would first need to start the oral version of the medication, and would be switched to the injectable form once tolerated. Initial studies looked into once monthly injections, however additional investigation is comparing injections every 60 days.
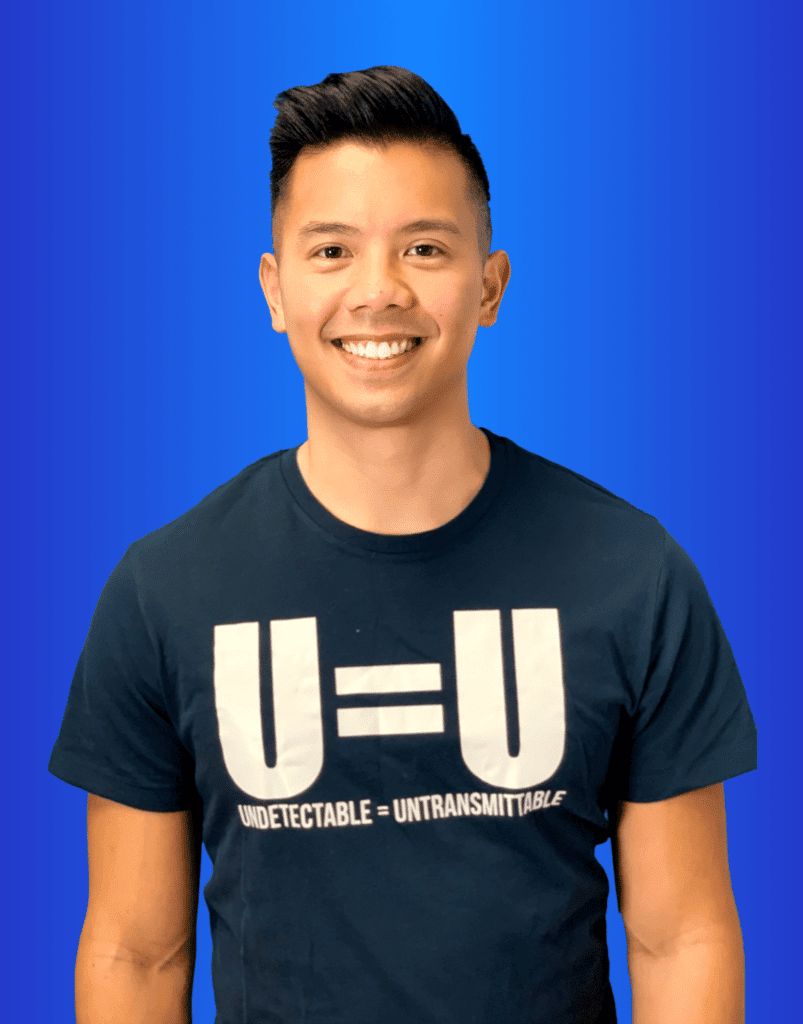
These breakthrough studies confirmed that individuals who were undetectable could not transmit the virus sexually to their partner. Undetectable=Untransmittable (U=U) means someone living with HIV who is undetectable can not transmit the virus to a partner through condomless sexual intercourse. Zero risk. This also applies to individuals who are virally suppressed with a viral load below 200 copies/mL.
Over several years, studies included thousands of cases of sexual intercourse between individuals who were undetectable and their negative partner. They found NO transmissions occurred between these partners. For more information check out our section on U=U.
These studies investigated if undetectable individuals living with HIV could effectively switch to a two-drug combination instead of their current treatment regimen. The study found the two-drug regimen remained effective once patients switched. As a result, a drug combination including dolutegravir and rilpivirine is available in Canada as a potential option for people living with HIV and undetectable to switch to.
This study evaluated the safety and effectiveness of using once-daily Descovy (emtricitabine 200 mg and tenofovir alafenamide 25 mg) for HIV pre-exposure prophylaxis (PrEP) vs Truvada (emtricitabine 200 mg and tenofovir disoproxil fumarate 300 mg). The study found it to be as effective with potentially improved safety (any rare risks with both medications are still quite low). The study focused on cis men and transgender woman at high risk for acquiring HIV so the results can not be applied to other genders. The US approved Descovy for PrEP-use and it is still waiting approval in Canada but may be prescribed “off-label” by your healthcare provider.
Studies have been underway investigating the use of antibodies to keep the HIV virus suppressed in people living with HIV. Some have shown that using antibodies kept the virus controlled for months after treatment in some people. Check out the links below on this type of treatment option and studies.
https://www.nih.gov/news-events/nih-research-matters/antibody-combination-suppresses-hiv
https://retrovirology.biomedcentral.com/articles/10.1186/s12977-018-0455-9
PrEP With Us
Most pay $0 With PrEPSaver
* The Injectable PrEP option is not part of our PrEPSaver Program.
Not sure if PrEP
is right for you?
Health is very personal and we feel it’s important to provide information to help you make a well-informed decision about PrEP. If you will ever have a possible exposure to HIV it is something to consider – especially if not always 100% sure of a sexual partner’s status.

